Criteria for nursing home care
All states have a medical center Medicaid program that provides health and wellness protection plus coverage for nursing home services. These services include space and board, nursing treatment, individual care and therapy services. Nursing Facility Medicaid may pay money for a stay in a nursing home in the event that you:
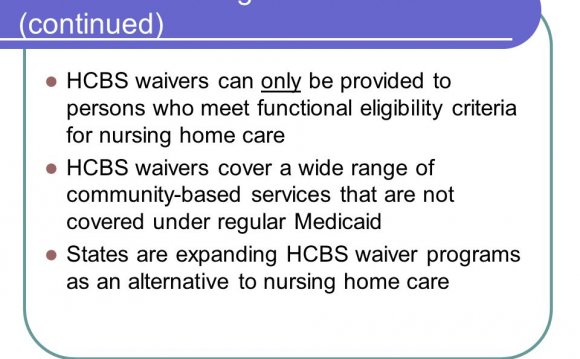
- require a nursing-home standard of treatment or meet medical home practical qualifications requirements; and
- have actually earnings and assets below particular directions.
Different says have actually different standards for determining whether you may need a medical home level-of-care, but generally speaking view your ability to work. Like, a state might examine whether you'll need assistance with activities of everyday living (i.e., basic each and every day tasks eg getting in and up out of bed, dressing, bathing, eating and with the bathroom).
While Medicare covers some competent nursing facility attention, it will just cover this maintain a limited length of time (up to 100 times in good results duration) in the event that you meet specific criteria. If you do not satisfy Medicare’s demands for the skilled medical center benefit or you have reached Medicare’s limit of covered skilled attention, Medicaid may purchase this treatment.
When you've got Nursing center Medicaid, you still have Medicare coverage when it comes to medical solutions you may need regardless of your nursing attention. If you ought to go directly to the medical center or need to go to a health care provider or specialist’s office, Medicare will pay first for the majority of of those medical solutions and Medicaid can pay second by covering your continuing to be costs, for instance the Medicare coinsurances, copayments and deductibles. Medicaid might also buy some medical services that aren't covered by Medicare, such as for example routine dental care.
Being qualify for Nursing Facility Medicaid, you will have to fulfill monetary instructions along with meeting useful qualifications recommendations. You could have income higher than you could have in the event that you would not require nursing home care whilst still being be eligible for Medicaid. Your state could have:
- greater Medicaid earnings directions for folks who require nursing home care than for people who don't; and/or
- a “spend-down” or “medically needy” system. Spend-down programs are meant for those that have income more than would usually qualify them for Medicaid coverage, but with medical expenditures that notably minimize their usable income.
Several things to understand if you're thinking of applying for Nursing center Medicaid:
- Nursing center Medicaid programs will start thinking about your spouse collectively when considering your earnings and possessions, but you'll manage to set-aside some your income and assets for your partner to keep. This amount will never be counted whenever you make an application for Medicaid.
- In the event that you be eligible for Nursing center Medicaid, you'll be able maintain a tiny bit of your revenue for a personal allowance. The total amount that you could hold on your own differs by state. Contact your neighborhood Medicaid company the precise quantity in your condition. You'll have to spend the rest of income towards the medical house.
- Medicaid has a “look-back duration” as much as 5 years. This means that Medicaid will look at any assets you have transferred in the past few years when determining eligibility and when Medicaid coverage will begin. If Medicaid determines which you have transferred possessions in breach for the Medicaid principles, it could penalize you by not purchasing part or all your nursing house stay.
- In the event that you own your home, make sure you speak with an elder legislation attorney about how precisely it'll influence your Medicaid eligibility and coverage. Depending on your position, the equity from your own home may count as an asset. When you no longer require long-term attention, or if you are deceased, your assets may be used to repay Medicaid the attention that it covered obtainable.













